Among patients with melanoma, those who received both ipilimumab and local peripheral treatments such as radiotherapy or electrochemotherapy had significantly prolonged overall survival compared with those who received only ipilimumab, according to a retrospective clinical study.
The study was published in Cancer Immunology Research, a journal of the American Association for Cancer Research.
Sebastian Theurich, MD, lecturer and physician-scientist in the Center of Integrated Oncology (CIO) at the University Hospital of Cologne, Germany.
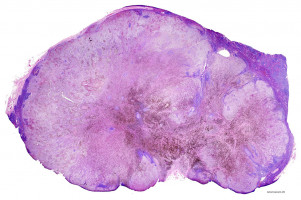
Ipilimumab is an immunotherapy that has revolutionised the treatment of malignant melanoma, a very aggressive type of skin cancer, according to Theurich.
About 20 percent of patients who receive ipilimumab achieve durable responses, which is a major advance compared with historic outcomes, but physician-scientists are looking for ways to increase the percentage of patients who gain long-term benefit from this immunotherapy, he added.
Currently, local peripheral treatments are not used to try and cure patients with malignant melanoma; rather, they are used to provide relief from symptoms caused by the melanoma tumours, explained Theurich.
Theurich and his colleagues analysed data from 127 patients with malignant melanoma who were treated consecutively at four cancer centers in Germany and Switzerland.
Eighty-two patients received ipilimumab only and 45 received ipilimumab and local peripheral treatment to relieve tumour-related symptoms.
Median overall survival for patients receiving ipilimumab and local peripheral treatment was 93 weeks, compared with 42 weeks for those receiving only ipilimumab.
After excluding patients with brain metastases from the analysis, because these patients were not distributed equally among the two treatment groups, the median overall survival benefit for those receiving ipilimumab and local peripheral treatment remained—117 weeks compared with 46 weeks for those receiving only ipilimumab.
“We found that adding local peripheral treatments, including external radiotherapy, electrochemotherapy, or internal radiotherapy, to systemic ipilimumab treatment doubled survival chances in our patient cohort and did not increase immune-related side effects,” said Theurich. “Importantly, this survival advantage seemed to overcome even traditional risk factors of poor outcomes. This suggests that this combination could be an option for all patients with malignant melanoma, and this is being tested in ongoing prospective clinical trials.”
“Our results are concordant with those previously reported for 29 patients treated in the United States with ipilimumab and local radiotherapy,” continued Theurich. “Having data from different parts of the world improves the validity of the results, especially if you deal with retrospective analyses. Moreover, all our patients were treated with the same dose of ipilimumab, whereas those in the previous study received varying doses because they were being treated in a dose- escalation clinical trial.”
“We were also able to begin to investigate the potential immunologic mechanism underlying the benefit of adding local peripheral treatment to ipilimumab,” added Theurich. “It seems that local peripheral treatments activate immune cells, which are then able to attack tumours at sites away from the local treatment site. However, we are investigating this further in prospective studies.”
Source: AACR
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.