After generating new brain tumour models, Cedars-Sinai scientists in the Board of Governors Regenerative Medicine Institute identified the role of a family of genes underlying tumour growth in a wide spectrum of high grade brain tumours.
"With these new genetic findings, our group of researchers plan to develop targeted therapeutics that we hope will one day be used treat patients with high grade brain tumours and increase their survival," said Joshua Breunig, PhD, a research scientist in the Brain Program at the Cedars-Sinai Board of Governors Regenerative Medicine Institute and lead author of the research study published in the journal Cell Reports.
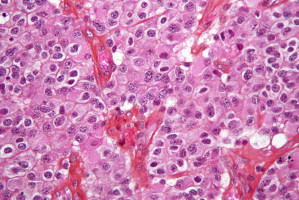
High grade brain tumours, known as gliomas, are difficult to treat with only a single digit five-year survival rate.
Most patients treated for primary gliomas develop into secondary gliomas, which are almost always fatal.
"Any given tumour can harbour a variety of different combinations of mutations," said Moise Danielpour, MD, Vera and Paul Guerin Family Chair in Pediatric Neurosurgery, director of the Pediatric Neurosurgery Program and the Center for Pediatric Neurosciences in the Maxine Dunitz Children's Health Center and last author on the study.
"Despite advances in radiation and chemotherapy, there are currently no effective curative regimens for treatment for these diverse tumours."
Researchers first modelled high grade brain tumours from resident stem cells inside the brain, using a cutting edge method of rapid modelling that can create up to five distinct tumour models within 45 minutes.
After effectively modelling high grade brain tumours, researchers identified the Ets family of genes as contributors to glioma brain tumours.
These Ets factors function to regulate the behaviour of tumour cells by controlling expression of genes necessary for tumour growth and cell fate.
When expression of the Ets genes is blocked, researchers can identify and strategize novel treatment therapies.
"The ability to rapidly model unique combinations of driver mutations from a patient's tumour enhances our quest to create patient-specific animal models of human brain tumours," added Danielpour.
Immediate next steps involve testing the function of each individual Ets factor to determine their specific role in tumour progression and recurrence after treatment.
References
Breunig, Levy, Antonuk et al. Ets factors regulate neural stem cell depletion and gliogenesis in Ras pathway-driven glioma. Cell Reports, 2015 July
Source: Cedars-Sinai Medical Center