Bowel cancer is often driven by mutations in one of several different genes, and a patient can have a cancer with a different genetic make-up to another patient’s cancer.
Identifying the molecular alterations involved in each patient’s cancer enables doctors to choose drugs that best target specific alterations.
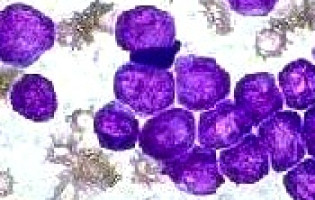
However, it is also becoming clear that while some cancers may be driven by a single gene mutation, individual tumours are often composed of groups of cancer cells, with each group having different molecular alterations from the others.
This is known as intra-tumour heterogeneity and it could have important consequences on the efficacy of therapies: in these “mixed” tumours, some tumour cell clusters might be sensitive to a targeted therapy while others are resistant.
Now, for the first time, a study published in the leading cancer journal Annals of Oncology has quantified the different mutational profiles of these clusters of cells in individual tumours in patients with bowel cancer that has spread to other parts of the body (metastasised).
The researchers in Italy have correlated the intra-tumour heterogeneity with the way the patients responded to specific drugs, such as cetuximab, an epidermal growth factor receptor (EGFR) inhibitor, which is a common treatment for patients with metastatic bowel cancer.
“Our study has shown there is a high degree of variability between different groups of cancer cells within one tumour, and we have been able to quantify this for the first time. The variability is likely to affect patients’ responses to drugs targeting specific genetic mutations, and our results also suggest that there is a subset of bowel cancer patients in whom resistance to anti-EGFR drugs may be driven by the complex mutational make-up of the tumour, rather than the molecular alteration of a single gene,” said Dr Nicola Normanno, Director of the Cell Biology and Biotherapy Unit and Director of the Laboratory of Pharmacogenomics, Centro di Ricerche Oncologiche di Mercogliano, at the Istituto Nazionale Tumori “Fondazione Giovanni Pascale” IRCCS, Naples, Italy, who led the study.
“It is difficult to predict when these findings can be translated into the clinic and we don’t want to create false expectations in the patients. However, we feel that by being able to quantify the relevant mutations, we will be able to improve personalised medicine for patients with bowel cancer and possibly with other types of cancers,” he said.
The researchers used “next generation sequencing”, which can provide information on several different genes in a single analysis, to investigate the mutational profiles of 182 tumour samples taken from patients in the CAPRI-GOIM trial – a multi-centre study of patients with metastatic colorectal cancer who were treated with chemotherapy and cetuximab, followed by a slightly different chemotherapy with or without cetuximab every two weeks when their cancer progressed.
To quantify the different mutational profiles in each tumour, the researchers developed a “Heterogeneity Score” (HS), which corresponded with the proportion of cancer cells carrying a specific mutation.
An HS of 100 suggests that all the cancer cells carry a specific mutation; an HS of less than 100 means that only a fraction of the cells are mutant; while an HS of more than 100 implies a structural variation in DNA involving either a gain of a mutant form of a gene or the loss of the “normal” (wild-type) form of the gene – a process known as copy number variation (CNV).
Dr Normanno said: “By using this scoring system, we found that different genes involved in bowel cancer behave in a different manner; for example, when a tumour has a mutation in the KRAS or NRAS genes, usually all the cells are mutant, whereas for other genes such as BRAF and PIK3CA only a fraction of tumour cells is mutant. In addition, we identified tumours that are clearly formed by multiple groups of cells with different molecular alterations.”
The average HS for mutations in the KRAS and NRAS genes was 87 and 103 respectively, suggesting that the majority of the cancer cells carried the mutations.
In contrast, the average HS for mutations in the BRAF and PIK3CA genes was 54 and 60, suggesting that only a fraction of cancer cells carried the mutant forms of the genes.
The researchers also found that 70% of patients with a KRAS HS of less than 33 responded to cetuximab, while only 46% of patients with a KRAS HS greater than 33 responded.
However, the length of time that both groups survived without their disease progressing was similar: 8 and 8.4 months respectively.
Patients in the “low KRAS” group had a higher frequency of additional mutations in the PIK3CA gene compared to those in the “high KRAS” group.
“This suggests that even if a patient has a lower HS score for KRAS and so responds well initially to EGFR-inhibitor treatments such as cetuximab, either other cancer cells take over to resist the treatment and drive the cancer, or another mutation such as PIK3CA continues to drive the cancer,” said Dr Normanno.
“This may mean that a treatment approach that uses a combination of drugs targeting different mutations may be more effective for these patients.”
The principal investigator of the CAPRI-GOIM trial is Professor Fortunato Ciardiello of the Second University of Naples.
Now, the researchers are planning to use next generation sequencing and their scoring system in large, prospective clinical trials of bowel cancer patients being treated with EGFR-targeting drugs, and in sub-groups of patients carrying specific mutations such as BRAF, in order to assess further the correlation between HS and patients’ response and outcome.
Source: Annals of Oncology
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.