Researchers at City of Hope®, one of the largest and most advanced cancer research and treatment organisations in the U.S. with its National Medical Centre named top 5 in the nation for cancer by U.S. News & World Report, have found that cell mutations are necessary but not always sufficient for tumours to form.
Instead, they suggest that additional risk factors that promote tumour growth, like chronic inflammation, are a key trigger for tumour formation.
The study findings, published this month in Cancer Discovery, answer a question that scientists have long asked: Are cell mutations alone — whether genetically inherited or acquired through lifestyle choices — enough to cause cancer?
“As a society, we have mostly focused on preventing mutations, like persuading people to stop smoking and to avoid water or food pollutants like plastics or heavy metals,” says Yun Rose Li, M.D., Ph.D., lead author of the paper and an assistant professor in City of Hope’s Department of Radiation Oncology and Department of Cancer Genetics and Epigenetics.
“Yet our study suggests an urgent need for cancer prevention strategies that target the biological mechanisms that trigger malignant tumours to develop and not merely focus on exposure to pollutants that cause mutations.”
For example, Dr. Li says, not all smokers get lung cancer.
She explains that while smoking likely acts as the initial carcinogenic event that causes cell mutations, those cells may then need a secondary inflammatory process to drive tumour formation.
Knowledge about what pushes tumours to develop could be used for comprehensive personalised risk assessment tests like those provided by City of Hope’s Cancer Screening & Prevention ProgrammeSM.
“We all have cells that will inevitably mutate, whether due to environmental mutations or random errors during cell division and tissue repair. From a public health standpoint, what people need to understand is that yes, it is important to avoid hazards, like smoking, that cause mutations, but it could be even more important to avoid situations that cause chronic inflammation — such as eating a high-fat diet or obesity — because inflammation is the match that ignites cancer,” says Dr. Li, who holds a joint appointment in The Bioinnovation and Genome Sciences Division at Translational Genomics Research Institute, part of City of Hope.
Other causes of chronic inflammation include excessive alcohol, lack of exercise, chronic stress, autoimmune disorders like rheumatoid arthritis or inflammatory bowel disease, and an imbalance of healthy and unhealthy microbes in your gut.
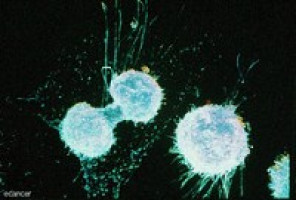
The researchers applied modern sequencing technologies to study inflammation-driven tumour models by replicating an experiment from the 1950s.
First, they applied two drugs, one to cause mutations followed by a second to create local inflammation, on skin tissue.
As expected, they found that tumours will form when the animal model’s skin was exposed to the first drug that causes thousands of cell mutations followed by the second agent.
The assumption based on their observations is that the immune system does not fix or clear out mutated cells, nor do these mutated normal cells naturally “die out.”
They applied whole genome sequencing to confirm that the primary mutations were caused by the addition of the first inflammation-causing carcinogen, which is essential to cancer development.
But neither agent on its own caused tumour formation.
They went one step further to show that even a single exposure as a foetus to a low dose of the first drug is sufficient to trigger the same mutation types that can be sufficient for tumour formation when the embryos become adults and are exposed to the inflammatory signal.
“What this means is that the initial exposure is sufficient in and of itself to cause all the necessary mutations that are required for tumour formation, but tumour development is reliant on the availability of this second signal or tumour promoter,” says Dr. Li, noting that while the work was done in skin cancer models, the findings can likely be applied broadly to many cancers, especially those that are age- and lifestyle-related.
“Mutated cells are still a lifetime risk factor. They're ticking time bombs lying latent, ready to be awakened.”
The researchers will now investigate the exact cellular mechanisms of tumour promotion.
For example, Dr. Li wants to explore how metabolic dysfunction can modify the epigenome, creating conditions that awaken latent mutated cells.
“By learning more about how tumour promotion works, my hope is that this work can have major implications for the development of new strategies for cancer prevention,” Dr. Li says.
Source: City of Hope