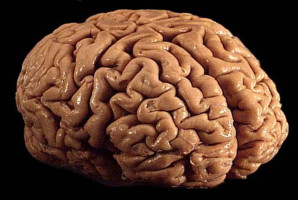
A drug developed at The University of Texas Health Science Centre at San Antonio (UT Health San Antonio) has been shown to extend survival for patients with glioblastoma, the most common primary brain tumour in adults.
Results of a trial led by the university revealed that a unique investigational drug formulation called Rhenium Obisbemeda (186RNL) more than doubled median survival and progression-free time, compared with standard median survival and progression rates, and with no dose-limiting toxic effects.
“As a disease with a pattern of recurrence, resistance to chemotherapies and difficulty to treat, glioblastoma has needed durable treatments that can directly target the tumour while sparing healthy tissue,” said Andrew J.
Brenner, MD, PhD, professor and chair of neuro-oncology research with Mays Cancer Centre at UT Health San Antonio.
“This trial provides hope, with a second phase under way and planned for completion by the end of this year.”
Brenner, who also is clinical investigator for the Institute for Drug Development at UT Health San Antonio and co-leader of its Experimental and Development Therapeutics Programme, is lead author of the trial’s study, titled, “Convection Enhanced Delivery of Rhenium (186Re) Obisbemeda (186RNL) in Recurrent Glioma: a multicenter, single arm, phase 1 clinical trial.” It published March 7 in the journal Nature Communications.
Other authors also are with Mays Cancer Centre, as well as UT Southwestern Medical Centre of Dallas, Case Western Reserve University, University of Texas MD Anderson Cancer Centre and trial sponsor Plus Therapeutics Inc.
(Nasdaq: PSTV), a clinical-stage pharmaceutical company receiving licence to the trial technology to investigate the treatment of central nervous system cancers.
Brenner said that the median overall survival time for patients with glioblastoma after standard treatment fails with surgery, radiation and chemotherapy is only about 8 months.
More than 90% of patients have a recurrence of the disease at its original location.
Rhenium Obisbemeda enables very high levels of a specific activity of rhenium-186 (186Re), a beta-emitting radioisotope, to be delivered by tiny liposomes, referring to artificial vesicles or sacs having at least one lipid bilayer.
The researchers used a custom molecule known as BMEDA to chelate or attach 186Re and transport it into the interior of a liposome where it is irreversibly trapped.
In this trial, known as the phase 1 ReSPECT-GBM trial, scientists set out to determine the maximum tolerated dose of the drug, as well as safety, overall response rate, disease progression-free survival and overall survival.
After failing one to three therapies, 21 patients who were enrolled in the study between March 5, 2015, and April 22, 2021, were treated with the drug administered directly to the tumours using neuronavigation and convection catheters.
The researchers observed a significant improvement in survival compared with historical controls, especially in patients with the highest absorbed doses, with a median survival and progression-free time of 17 months and 6 months, respectively, for doses greater than 100 grey (Gy), referring to units of radiation.
Importantly, they did not observe any dose-limiting toxic effects, with most adverse effects deemed unrelated to the study treatment.
“The combination of a novel nanoliposome radiotherapeutic delivered by convection-enhanced delivery, facilitated by neuronavigational tools, catheter design and imaging solutions, can successfully and safely provide high absorbed radiation doses to tumours with minimal toxicity and potential survival benefit,” Brenner concluded.
Information on Phase 2 of the ReSPECT-GBM trial, which is actively enrolling patients, can be found here.
Link to full study: https://www.nature.com/articles/s41467-025-57263
Source: University of Texas Health Science Center at San Antonio
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.