A preclinical study led by a faculty member at Roswell Park Comprehensive Cancer Center shows that gilteritinib, a targeted cancer treatment, can strengthen chimeric antigen receptor (CAR) T-cell immunotherapy in two high-risk paediatric leukaemias that have poor survival rates — FLT3-mutated acute myeloid leukaemia (AML) and KMT2A-rearranged acute lymphoblastic leukaemia (ALL).
Lisa Niswander, MD, PhD, Assistant Professor of Oncology in the Department of Pediatric Oncology, delivered the results in an oral abstract session at the 66th annual meeting of the American Society of Hematology (ASH) in San Diego, California.
Both types of leukaemia are characterised by abnormal levels or overactivity of FLT3, a protein on the surface of some leukaemia cells. “Children with FLT3-mutant AML and infants with KMT2A-rearranged ALL are in desperate need of new therapies to minimise toxicities and improve long-term remission,” says Dr. Niswander. “Our preclinical studies take a two-pronged approach to targeting FLT3-expressing leukaemias, by combining CAR T-cell immunotherapy and the FLT3 inhibitor gilteritinib.”
Lisa Niswander, MD, PhD, Assistant Professor of Oncology in the Department of Pediatric Oncology,
The investigators found that, compared with administering the two therapies separately, they achieved superior destruction of leukaemia cells by combining gilteritinib, a type of drug called a tyrosine kinase inhibitor, with FLT3 CAR T-cell immunotherapy in preclinical models of FLT3-mutant AML and KMT2A-rearraranged ALL.
Initially the team hypothesised that the improved outcomes were due to the combined action of each distinct type of therapy working individually to target the leukaemia cells, but they made a surprising discovery.
“While we anticipated that these therapies would directly target leukaemia, we also observed that gilteritinib directly increases the number of CAR T cells and improves the eradication of leukaemia cells, providing enhanced and sustained anti-leukaemia activity,” explains Dr. Niswander. “We’re excited to share this work at ASH, and we anticipate that these findings will lay the foundation for a promising translational strategy for future clinical investigation.”
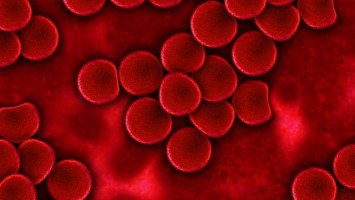
CAR T-cell therapy centres on a patient’s own T cells, which are part of the normal immune system and can be collected from a patient’s blood and engineered in the laboratory to recognise a specific protein on the surface of cancer cells.
The engineered CAR T cells are then multiplied and returned to the patient, where they attach themselves to — and kill — leukaemia cells.
In preclinical work, Dr. Niswander and her colleagues previously developed CAR T cells that target FLT3 and demonstrated that they could be effective against those types of leukaemia.
FLT3 contains activating mutations in 20-30% of paediatric AML patients and is abnormally highly expressed in KMT2A-rearranged ALL.
The majority of infants under 12 months of age with ALL have KMT2A-rearranged leukaemia, which confers a poor prognosis, with long-term survival rates under 60%.
Gilteritinib (brand name Xospata) is a targeted small-molecule drug that prevents leukaemia cells from surviving and multiplying, by inhibiting signalling of multiple receptor tyrosine kinases, including FLT3. It is FDA-approved for the treatment of adult patients with recurrent or treatment-resistant FLT3-mutated AML .
Dr. Niswander and her colleagues conclude that gilteritinib co-therapy can also strengthen the power of alternative leukaemia-targeting CAR T-cell products, highlighting the potential of gilteritinib to enhance the effectiveness of other CAR T-cell immunotherapies already in clinical use in paediatric patients.
The research team includes collaborators from Children’s Hospital of Philadelphia/University of Pennsylvania School of Medicine and the University of Colorado Anschutz Medical Campus.