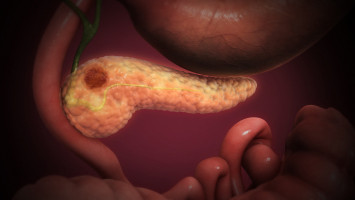
A new study published today in JAMA Network Open by an international cohort of researchers provides the latest data on the effectiveness of treating pancreatic cancer patients with chemotherapy (with or without radiation therapy) before surgery to remove a tumour.
The study focuses specifically on pancreatic adenocarcinoma patients.
The research found that after treatment and surgery, nearly five percent of patients had no detectable cancer cells left in the area where the tumor was, achieving a pathological complete response (pCR).
“PCR means that the cancer has responded extremely well to the treatment, leaving no evidence of cancer in the area examined. Although pCR does not mean someone is cured, patients who have pCR tend to live longer,” said the paper’s senior author Marco Del Chiaro, MD, PhD, division chief of surgical oncology at the CU Cancer Center on the University of Colorado Anschutz Medical Campus.
The study found those with pCR had a 5-year survival rate of 63 percent, whereas those without it had a rate of only 30 percent. This means the survival rate doubles with pCR. These results are helpful to inform patients after surgery, providing information on their prognosis.
“This increase is a big deal for a disease like pancreatic cancer where progress and treatments have gradually improved over the years but is still much lower than other cancers,” adds Del Chiaro.
The paper also goes into detail about the factors that contribute to pCR.
The researchers assessed nearly 1,760 patients with pathology-proven localised pancreatic adenocarcinoma who underwent resection after two or more cycles of chemotherapy (with or without radiotherapy) in 19 centers from eight countries and three continents.
They found several factors associated with achieving pCR, including the specific chemotherapy regimens used before surgery, radiation therapy and the way the cancer responded to treatment based on its anatomy and biology.
“Our ultimate goal is to improve the selection of treatment for patients and enhance prognostic accuracy. We hope this research paper can help oncologists understand the predictors that make patients more likely to achieve pCR, and improve survival, including the biological factors that make a tumour more favourable for surgery,” said first author Thomas Stoop, MD, who works at the Amsterdam University Medical Center and former research fellow at the CU Anschutz Medical Campus in the field of pancreatic cancer surgery.
The findings suggest that tailoring treatment based on these factors could be beneficial. However, they note that these factors might only apply to some patients uniformly.
For instance, while one treatment method (SBRT) was associated with achieving pCR, it was not associated with increase in overall survival rate.
This highlights the complexity of treatment decisions and the need for further research to validate these findings and understand their broader applicability across different patient populations.
“Although there are a lot of complexities in understanding and improving treatments for pancreatic cancer, I’m hopeful for the future and this study is part of the reason why. Researchers working together worldwide to provide more in-depth data strengthens our ability as doctors and researchers to provide better treatment plans and breakthroughs to help our patients,” said Del Chiaro.