Breast cancer is the most common cancer affecting women in Singapore.
Treatment is multimodal and often involves surgery to remove the cancer and lymph nodes involved.
Adjuvant therapy, given after the initial treatment, is used to irradiate and destroy micrometastases, which are cancer cells in the blood stream or lymphatics, to decrease recurrence.
This form of therapy is subdivided into local (radiotherapy) and systemic therapy (endocrine therapy, chemotherapy and targeted therapy).
Studies have shown that patient satisfaction has increased with breast conserving therapy (BCT) where only the tumour and a margin is removed from the body post mastectomy, compared to full mastectomy alone, which removes all parts of the breast.
For BCT, radiotherapy has to be administered after lumpectomy, which removes other abnormal tissue from the breast and some normal tissue around it.
However, in radiotherapy, photon beams, which are administered externally, are used to induce tumour damage.
As the breast sits above the chest wall, lungs and heart, there is a small risk of toxicity to the skin, lung, heart and remaining breast tissues, which can lead to fat necrosis and the hardening or distortion of the breast.
Furthermore, radiotherapy is administered daily over 3 to 5 weeks, and patients with more advanced forms of breast cancer also require radiotherapy despite undergoing mastectomies.
To avoid the side effects and improve quality of care for breast cancer patients, a multidisciplinary team comprising medical researchers, bioengineers and clinicians from the National University of Singapore (NUS) and National University Hospital (NUH), led by Assistant Professor Daniel Teh from the Department of Ophthalmology and Anatomy at the Yong Loo Lin School of Medicine, NUS (NUS Medicine) and Professor Zhang Yong from the Department of Biomedical Engineering in the College of Design and Engineering, NUS,have, successfully delivered tumour-selective light treatment to breast cancer cells.
This mode of treatment, known as photodynamic therapy, was shown to be effective in breast cancer preclinical models in their recent publication in ACS Nano.
Unlike usual forms of photodynamic therapy, this treatment does not need wires for powering.
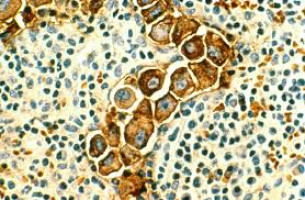
The driving reasons for the success of this discovery are two-fold: firstly, breast cancer cells can take up an FDA-approved light-activated drug known as 5-aminovulenic acid (5-ALA), which can be administered intravenously to patients.
When activated by light in the blue spectrum, this drug is capable of unleashing a tumour killing effect, making its effects localised, without killing cells in other regions.
As the blue light has poor tissue penetration properties and is unable to reach deeper tissues when applied on the skin surface, the team worked to improve the delivery of light to tumours that lay in tissues deeper in the skin.
The researchers engineered a biologically compatible silicone breast implant loaded with nanoparticles that can be activated by highly tissue-penetrant near-infrared light.
This can be converted into visible light needed for the activation of 5-ALA.
The implant can be inserted into the tumour cavity after complete surgical removal of the tumour in its original place.
After the patient recovers from surgery, 5-ALA can be administered intravenously, and the implant can be activated by simply shining light on the surface of the breast.
The nanoparticles, known as up conversion nanoparticles (UCNPs), are quickly opening up a field known as ‘photo-nanomedicine’ for their unique properties.
The UCNP-impregnated silicone implant designed by the NUS team has several advantages.
As its matrix material is silicone, its mouldable nature and soft consistency enables it to be used for partial and total breast reconstruction.
The implant is especially useful, as its biocompatible nature allows it to be left in its original place for long periods, allowing photodynamic treatment to be delivered on-demand, even when treatment is delayed.
This feature allows treatment to take place in the setting of local recurrence.
“This discovery has the potential to significantly augment existing breast cancer therapies. Being able to selective destroy tumour cells without inducing adjacent tissue damage confers a significant advantage in cancer treatment. While it will probably not replace existing mainstream treatment modalities, it may still indirectly lead to a reduction in chemotherapy and/or radiation dosage by improving local tumour control,” said Assistant Professor Teh.
“This discovery has potential to change the treatment of breast cancer, improving aesthetic outcomes of patients while still preserving oncological safety. Furthermore, the implant allows more tissue to be removed with improved rates of tumour clearance and can act as a “safety net” against local recurrences,” commented Assistant Professor Celene Ng, Consultant from the Division of General Surgery (Breast Surgery), Department of Surgery, NUH.
This photodynamic therapy is a useful addition to the arsenal of existing therapies for breast cancer.
When used alongside conventional treatments, photodynamic therapy can possibly reduce disease burden and indirectly help to lessen treatment-related toxicities with conventional therapies.
Article: SIRIUS, ultra-scintillating upconversion breast implant for remote orthotopic photodynamic therapy
Source: National University of Singapore, Yong Loo Lin School of Medicine