An experimental antibody treatment largely prevented a bone marrow transplant complication called graft versus host disease (GVHD) in the intestines, without causing broad immune suppression, in a preclinical study led by researchers from Penn Medicine and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and published today in Science Translational Medicine.
Even when a bone marrow transplant cures leukaemia or lymphoma, GVHD—in which T cells in the donor graft attack the recipient’s own tissues—can still be fatal.
The condition is among the leading causes of death and long-term adverse health consequences associated with bone marrow transplants.
Senior co-corresponding authors Ivan Maillard, MD, PhD, a professor of Medicine and vice chief for research in Haematology at the Perelman School of Medicine at the University of Pennsylvania, and Leslie S. Kean, MD, PhD, a professor of Paediatrics at Harvard Medical School and director of Pediatric Stem Cell Transplant at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, along with lead author Victor Tkachev PhD, an assistant professor of Surgery at Mass General Brigham, have long sought to prevent this fatal complication.
Their study helps pave the way for human clinical trials of the new treatment.
“We found that just a single dose of antibodies to block the Notch signalling pathway, given immediately before the transplant, was able to prevent gastrointestinal GVHD, without impairing immune function in the rest of the body,” Maillard said.
“The timing was critical. Intervening before any symptoms of GVHD appear made the long-term protection possible.”
Maillard and colleagues found in prior studies that the GVHD-causing activity of donor immune cells—especially T cells—requires a signalling pathway called the Notch pathway.
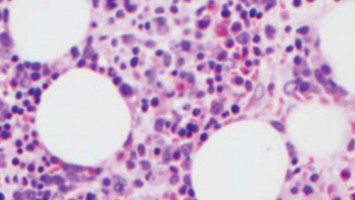
In experiments with mouse models of GVHD, the researchers found that blocking a particular Notch activator—known as DLL4—was very effective at preventing GVHD when administered within the first days after transplantation: It stopped donor T cells from infiltrating and attacking the intestines, a major site of severe GVHD, yet did not block the T cells’ infection- and cancer-fighting capabilities.
In this study, Maillard and his lab teamed up with Tkachev, Kean, and colleagues, to test the anti-DLL4 strategy in a large animal model of GVHD, which the Boston researchers developed to better simulate the human immune system and the effects of GVHD treatment.
They confirmed that the Notch pathway involvement in GVHD was conserved across species, and that just a single dose of the DLL4-blocking antibody given immediately before transplant greatly increased survival and prevented signs of GVHD in the intestines without causing global immunosuppression.
The researchers traced the anti-DLL4 antibodies’ specific protection against gastrointestinal GVHD to the reduction of an adhesion molecule that normally promotes T-cell migration to the intestines.
The successful test in multiple preclinical models opens the way for initial clinical trials, now being planned at Penn Medicine and Dana Farber/Boston Childrens, the researchers said.
“If this new, more targeted strategy for preventing GVHD is successful in clinical trials, it might allow us to extend the use of bone marrow transplants to higher risk patients who are not currently eligible for a traditional transplant,” said Kean.
“This unique approach could allow us to thread the needle between efficacy and the downsides of global immunosuppression caused by other GVHD treatments.”