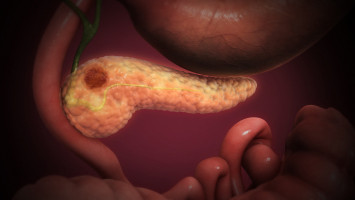
Researchers have discovered a molecular pathway critical to the initiation of pancreatic tumours.
The mechanism could also contribute to the disease’s high resistance to chemotherapy and its propensity for metastasis.
The study, published on January 16, 2023 in Nature Cell Biology, found that pancreatic tumour-initiating cells must first overcome local ‘isolation stress’ by creating their own tumour-promoting microenvironment, and then recruit surrounding cells into this network.
By targeting this tumour-initiating pathway, new therapeutics could limit the progression, relapse and spread of pancreatic cancer.
Pancreatic cancer is one of the most lethal cancers, notoriously resistant to treatment.
Almost all patients experience cancer recurrence or metastasis.
In the early stages of tumour formation, cancer cells (those with cancerous mutations, called oncogenes) experience a loss of adhesion to other cells and the extracellular matrix — the web of macromolecules that encase and support all cells.
This isolation leads to a local lack of oxygen and nutrients.
Most cells do not survive such isolation stress, but a certain group of cells can.
Tumour-initiating cells (TIC) play a major role in the formation, recurrence and metastatic spread of tumours.
What sets them apart from other cancer cells is their resilience to these early substandard conditions.
Like cacti in a desert, they can adapt to the harsh environment and set the scene for further tumour progression.
“Our goal was to understand what special properties these tumour-initiating cells have and whether we can control the growth and spread of cancer by disrupting them,” said senior study author David Cheresh, PhD, Distinguished Professor and vice chair of the Department of Pathology at UC San Diego School of Medicine and a member of the UC San Diego Moores Cancer Centre.
To answer these questions, first author Chengsheng Wu, PhD, a postdoctoral fellow in Cheresh’s lab, subjected pancreatic cell lines to various forms of stress, including low oxygen and sugar levels.
He then identified which cells could adapt to the harsh conditions and observed which genes and molecules were modified in these cells.
The stress-tolerant tumour-initiating cells showed reduced levels of a tumour-suppressive microRNA, miR-139-5p.
This in turn led to the upregulation of lysophosphatidic acid receptor 4 (LPAR4), a G-protein-coupled receptor on the cell surface.
“LPAR4 is not normally found on happy cells, but it gets turned on in stressful environments to help the cells survive, which is particularly advantageous for tumour-initiating cells,” said Cheresh.
The researchers found that LPAR4 expression promoted the production of new extracellular matrix proteins, allowing the solitary cancer cells to start building their own tumour-supporting microenvironment.
The new extracellular matrix was particularly rich in fibronectin, a protein that binds to transmembrane receptors called integrins on surrounding cells.
Once the integrins on these cells sensed the fibronectin, they began signalling the cells to express their own tumour-initiating genes.
Eventually, these other cells were recruited into the fibronectin matrix laid by the tumour-initiating cells and a tumour started to form.
“Our findings establish a critical role for LPAR4 in pancreatic tumour initiation, and a likely role in other epithelial cancers, such as lung cancer,” said Cheresh. “It is central to tumour-initiating cells’ ability to overcome isolation stress and build their own niche in which tumours can form.”
But isolation stress is not the only way this signalling pathway can be triggered, the researchers said.
Chemotherapy drugs are also designed to put cancer cells under stress.
Indeed, Cheresh’s team found that treating cultured tumour cells and pancreatic tumours in mice with standard-of-care chemotherapeutics also led to the upregulation of LPAR4.
The researchers said this might explain how such tumour cells could develop a stress tolerance and resistance to the drugs.
Further experiments also showed that using integrin antagonists to block cells’ ability to utilise the fibronectin matrix reversed the stress tolerance benefit of LPAR4 expression.
Thus, the authors suggest targeting the LPAR4 pathway or disrupting the fibronectin/integrin interaction could be effective in preventing the growth, spread and drug resistance of pancreatic tumours.
“We can think of tumour-initiating cells as being in a transient state that can be induced by different stressors, so our clinical goal would be to prevent oncogenic cells from ever entering this state,” said Cheresh. “Now that we've identified the pathway, we can assess all the different ways we can intervene.”
The researchers suggested a new drug targeting this pathway could be used as a prophylactic in patients at high risk of developing the disease, or to prevent new tumours from forming in cancer cases with a high likelihood of metastasis.
Pairing the new drug with existing chemotherapeutics that put stress on mature tumour cells could also mitigate the effects of drug resistance and make cancer treatments more effective, authors said.
“Treating cancer can feel a little like whack-a-mole,” said Cheresh, “but if we have two or three hammers and we know where the moles are going to pop up next, we can beat the game.”
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.