Natural killer (NK) cells derived from cord blood that were activated and complexed with a CD30/CD16A bispecific antibody elicited an 89 percent overall response rate in patients with relapsed or refractory CD30+ lymphoma, according to results from a phase I/II clinical trial presented at the AACR Annual Meeting 2022, held April 8-13.
“We were favorably surprised by the quality of tumor responses in patients who had resistant lymphomas, some of whom were in a very poor condition at enrollment,” said Yago Nieto, MD, PhD, a professor of medicine in the Department of Stem Cell Transplantation and Cellular Therapy at The University of Texas MD Anderson Cancer Center, who presented the study.
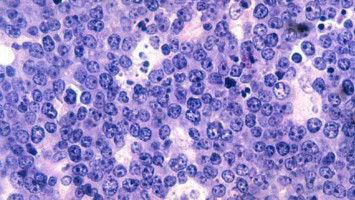
CD30 is a receptor expressed on certain cells in many Hodgkin lymphomas and some non-Hodgkin lymphomas, and its activation promotes the growth of cancer cells. The current standard of care for relapsed CD30+ lymphomas is brentuximab vedotin (Adcetris), an antibody-drug conjugate that delivers a toxic cytoskeleton destabilizing agent to cells expressing CD30. However, not all tumors respond.
“Relapsed CD30+ lymphoma is successfully treated, in many cases, with brentuximab vedotin and, in the case of Hodgkin lymphoma, checkpoint inhibitors as well,” Nieto said. “But if these treatments fail, these patients’ tumors become extremely resistant to killing, and patients are left with very few effective therapeutic options.”
To address this problem, Nieto and colleagues utilized a bispecific antibody that binds to CD30 on lymphoma cells and CD16A on natural killer cells. The antibody, innate cell engager AFM13, acts as a bridge between the two cell types, helping the natural killer cells more effectively fight the cancer.
Prior studies with AFM13 showed preliminary efficacy in clinical trials of patients with Hodgkin lymphoma, T-cell lymphoma, and peripheral T-cell lymphoma. In preclinical studies, however, Nieto’s colleague Katy Rezvani, MD, PhD, also a professor of medicine in the Department of Stem Cell Transplantation and Cellular Therapy at MD Anderson, found that linking AFM13 to cord blood-derived activated NK cells prior to infusing them into mice was more effective than treating mice with AFM13 or the unlinked NK cells alone.
“We wanted to evaluate the tolerability and activity of this novel adoptive cellular immunotherapy using allogeneic natural killer cells, whose intact killing capacity can be further increased by cytokine pre-activation and whose numbers can be largely expanded in the lab,” Nieto said.
Nieto and colleagues isolated NK cells from cord blood, a readily available source of adaptable hematopoietic cells that have been shown to produce fewer immunological side effects than cells from peripheral blood.
The researchers used a mixture of cytokines to activate the cells into a memory-like state, making them more persistent and effective. They expanded the cells in culture and complexed them with AFM13.
So far, the researchers have recruited 22 patients with relapsed CD30+ lymphoma, all of whom had received prior treatment with brentuximab vedotin, and most of whom had received a stem cell transplant. Patients were treated with AFM13-NK cell complexes following immune cell depletion using fludarabine and cyclophosphamide.
They received two cycles of 1 million cells/kg (three patients), 10 million cells/kg (three patients), or 100 million cells/kg (13 patients), with the highest dose selected as the recommended phase II dose. Patients were given additional infusions of AFM13 alone seven, 14, and 21 days after treatment with the complexed cells.
Across all dose levels, 53 percent of patients experienced a complete response, 37 percent experienced a partial response, and 11 percent had progressive disease. Notably, among the 13 patients treated at the recommended phase II dose, the overall response rate was 100 percent, including eight complete responses and five partial responses.
At a median follow-up of 11 months across all dose levels, the progression-free survival rate was 53 percent, and the overall survival rate was 79 percent. Apart from the expected hematological toxicity resulting from pre-infusion immune cell depletion, the researchers observed no adverse events from the natural killer cells and only one adverse event of grade 3 or higher from a subsequent AFM13 infusion.
“Our preliminary results indicate excellent tolerability and high activity and warrant further investigation of this approach,” Nieto said. “We hope that this new therapeutic option can potentially be used as a bridge to stem cell transplantation or perhaps even as a curative treatment and will bring hope to this patient population with a large unmet need.”
Limitations of this study include a relatively short duration of follow-up and limited information about the durability of response after two cycles.
Funding of this study was provided by Affimed Therapeutics. Nieto is on the advisory board for Affimed and receives research funding from Affimed, Astra Zeneca, Bio Secura, and Novartis.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.