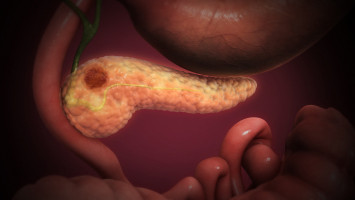
Pancreatic ductal adenocarcinoma (PDAC) is the most common form of pancreatic cancer.
The disease is almost always fatal, with a 10-year survival rate of around 1 percent.
The prognosis is especially poor for a subgroup of these tumours known as mesenchymal PDAC subtype, where even the strongest combination chemotherapies do not improve the poor clinical outcomes.
Mesenchymal PDAC is also unresponsive to modern immunotherapies such as checkpoint blockades.
There are different reasons for this.
First, there are few features on the tumour cell surface that enable immune T-cells to identify them as “foreign”.
Second, the nature of the microenvironment does not allow therapeutically active T-cells to infiltrate the cancer.
We therefore call it an immunologically “cold” tumour,” says Dieter Saur, Professor of Translational Cancer Research at the Technical University of Munich (TUM).
Saur is one of the scientists working at the Munich partner site of the German Cancer Consortium (DKTK) at the University hospital Klinikum rechts der Isar.
If this microenvironment could be reprogrammed to improve T-cell infiltration of the tumour, immunotherapy treatments would have a better chance of success.
The scientists explored this hypothesis in a series of preclinical experiments in human pancreatic cancer cells and in mice.
The drug trametinib showed early promise with cancers that activate the RAF-MEK-ERK signalling pathway.
Because pancreatic cancers of the mesenchymal subtype show the highest activation of this pathway, it appeared likely that a drug that inhibits this pathway could offer therapeutic benefits.
Experiments showed, however, that treatments with trametinib alone were insufficient.
The researchers therefore conducted high-throughput screening of 418 drugs on human PDAC cell cultures as well as cancerous cells from mice to find out whether one of them would improve the therapeutic effect of trametinib.
They discovered that nintedanib, a drug already approved for lung fibrosis treatment, stimulated T-cell infiltration when used in combination with trametinib.
“The combination of the two drugs led to cell cycle arrest and the death of cancerous cells. They also changed the microenvironment of the tumour,” says Dieter Saur, explaining the underlying mechanism.
Next the researchers investigated whether these changes could sensitize mesenchymal pancreatic carcinomas for treatment with immune checkpoint inhibitors.
This question was explored through experiments on mice transplanted with tumour cells of PDAC subtypes.
“The responses we observed in mice showed us that the anti-PD-L1 immunotherapy improved the effect of the combination treatment with trametinib and nintedanib,” says Chiara Falcomatà, the first author of the study. “The triple treatment significantly improved the response of the tumour, leading to a clear survival advantage of the highly aggressive mesenchymal PDAC subtype.”
The results represent an important first step toward targeted treatment of mesenchymal PDAC, for which there are currently no efficient therapeutic options.
The researchers believe that the combination treatment may also have the potential to create anti-tumour immunity with other cancer types, resulting in improved therapeutic outcomes.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.