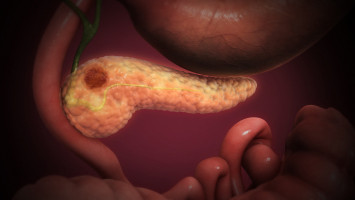
Research led by scientists at the Jonsson Comprehensive Cancer Center (JCCC) at UCLA provides new insights into molecular “crosstalk” in pancreas cancer cells, identifying vulnerabilities that could provide a target for therapeutic drugs already being studied in several cancers.
This interdisciplinary research was led by a team of JCCC investigators, Dr. Caius Radu, an expert in cancer cell metabolism, and Dr. Timothy Donahue, a pancreas cancer surgeon and an expert in pancreas cancer biology.
“Pancreatic ductal adenocarcinoma, which is highly resistant to current therapies, is expected to become the second most common cause of cancer-related deaths in the United States within this decade,” said senior author Caius Radu, MD, a researcher at Jonsson Comprehensive Cancer Center at UCLA and Professor in the Department of Molecular and Medical Pharmacology at UCLA. “Results of this study increase our understanding of the inflammatory microenvironment within these tumours and suggest targeted pharmacological strategies that could be employed to leverage this hallmark feature of pancreas cancer by current treatments.”
The preclinical research, using tumour cells from patients and cell line-derived xenograft tumours, was published online at Cell Reports.
It centres on STING-driven type I interferon, an immune system signalling molecule that impairs cancer cell proliferation in lab studies but tends to have the opposite effect in clinical practice, where tumour cells adapt to them and often become resistant to treatment with radiation, chemotherapy and immune checkpoint blockade.
Interferons are produced in immune and other cells, including some types of cancer cells.
“We determined that a subset of PDAC tumours exhibit an intrinsic interferon response that has not been modelled by standard cell culture conditions. Using several advanced techniques, we found that interferon signalling causes the tumour cells to rely on a specific signalling pathway for survival. However, if we inhibit a protein called ATR, which plays an important role in this signalling pathway, we can cause catastrophic damage to the cancer cells’ DNA and induce programmed cell death,” said Evan Abt, a postdoctoral researcher in Dr. Radu’s lab and co-first author of the article with Thuc Le, adjunct assistant professor in Molecular and Medical Pharmacology, and Amanda Dann, MD, a resident in surgery at the UCLA David Geffen School of Medicine.
Results suggest that new small molecule drugs that inhibit ATR and are being studied for treatment of several cancers, including PDAC, could be used in combination with interferon “amplification” to thwart the tumour cells’ ability to escape.
The researchers defined a series of molecular interactions leading to a cascade of intracellular events.
Through its influence on several genes, interferon alters the metabolic processes supporting the foundation of the cancer cells’ DNA, reducing the supply of biochemical building blocks needed for the DNA to survive.
To compensate, the cancer cells rely on a signalling pathway – the replication stress response signalling pathway – that can enable threatened DNA to survive, largely through the influence of ATR.
Dr. Donahue said one potential intervention deserving further exploration, according to results of the study, therapy that activates another signalling pathway, called STING.
“STING activation induces interferon signalling in PDAC cells and triggers ATR activation,” he said. “This strategy would enhance the attack brought about through interferon signalling while preventing escape through the collateral pathway by shutting it down with ATR-inhibiting drugs.”
Source: University of California - Los Angeles Health Sciences
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.