Utah researchers report significant new insights into the development of blood cancers.
In work published today in Blood Cancer Discovery, a journal of the American Association for Cancer Research, scientists describe an analysis of published data from more than 7,000 patients diagnosed with leukaemia and other blood disorders.
Their findings provide new clues about mutations that may initiate cancer development and those that may help cancer to progress.
The researchers sought to identify mutation hotspots, or frequent changes in specific locations of the cancer patients' genetic information.
The researchers then used these hotspots to look for whether the same mutations were present in the DNA data of more than 4,500 people who were not known to have a cancer diagnosis.
They found that approximately 2 percent of these presumably healthy participants had, at low levels, mutations identical to those frequently observed in the cancer patients.
"Understanding how a disease develops is greatly benefited by studying persons who are currently healthy but are on a trajectory for disease onset," said Clint Mason, PhD, assistant professor of paediatrics at the U of U, who specialises in cancer genomics and bioinformatics and led the study.
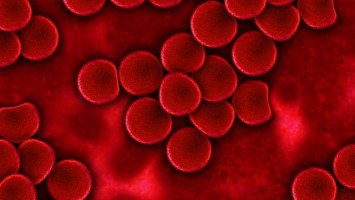
Mutations occur throughout the 3 billion bases of DNA that are present in human cells.
Many will have no impact on health, yet certain mutations may cause or support development of diseases, including cancer.
Therefore, scientists are working to discern which mutations have a significant impact on health.
In this study, the researchers sought to understand which mutations are most frequently present in adults and children both with and without blood cancers.
They hope this information may illuminate an understanding of these cancers, and further, may potentially be used to identify people who are progressing towards cancer.
The team of researchers consisted nearly entirely of University of Utah (U of U) faculty and students. Mason was joined by co-first authors Julie Feusier, PhD, a trainee in the department of human genetics and now a postdoctoral fellow at Huntsman Cancer Institute, and Sasi Arunachalam, PhD, a postdoctoral fellow at Huntsman Cancer Institute and now a research associate at St. Jude Children's Research Hospital, in performing analyses along with other co-authors.
For the first part of the study, the researchers completed a large data mining analysis to examine published data from 48 cancer studies that reported mutations present in persons who were being diagnosed with leukaemia or other haematologic malignancies.
Across the 7,430 paediatric and adult cancer patients of those studies, 434 DNA locations were identified as frequently mutated.
Then, in a subsequent analysis of many terabytes of publicly available genetic data, the researchers identified these same cancer-relevant mutations at low levels among 83 of the 4,538 persons who were presumably free from cancer.
"When identical mutations are found to be present in a small percentage of blood cells of a healthy person, it may indicate that something abnormal has begun to occur," explained Mason.
This abnormal process (known as clonal haematopoiesis) has previously been found to be increasingly common as people age. As a result, researchers generally focus on the study of adults when investigating this phenomenon.
Yet in this study, in addition to adults, the researchers analysed data from 400 children who were likely to be free from cancer. They found preliminary evidence that early cancer mutations could be detected in this age group.
In an accompanying commentary, to be published by Blood Cancer Discovery in its "In the Spotlight" section, Barbara Spitzer, MD, and Ross Levine, MD, of the Memorial Sloan Kettering Cancer Center, wrote, "This work demonstrates the first evidence that [clonal haematopoiesis] is observed in children outside of those with advanced malignancies."
They further commented, "This expansion of the range of haematologic malignancy hotspot mutations goes beyond an improved understanding of the molecular repertoire of haematologic malignancies.
More complete knowledge of relevant mutations may increase our detection of patients at highest risk for malignant transformation."
Finding a low-level mutation identical to one that is frequently present at cancer diagnoses could be alarming to a currently healthy person screened for such events.
But fortunately, because cancer frequently requires multiple mutations to be present in a sizeable fraction of cells, most persons with a single low-level mutation are not likely to develop cancer for many years or decades--if they develop cancer at all.
Large longitudinal studies are needed to identify the timeframe over which specific mutations or combinations of mutations accelerate progression to cancer.
The Utah researchers next hope to determine the stability of mutations identified at younger ages. This will give a preliminary glimpse into their potential to serve as biomarkers for those having greatest risk of cancer.
Future intervention studies will require such an identification.
"Our goal has been to help fill in gaps in the understanding of cancer development so that future prevention work can take place more quickly and effectively," said Mason.
"We are grateful to have been able to contribute a few puzzle pieces to that monumental effort."
Source: Huntsman Cancer Institute