Knocking out a protein known to stifle T cell activation on CAR T cells using the CRISPR/Cas9 technology enhanced the engineered T cells' ability to eliminate blood cancers, according to new preclinical data from researchers in the Perelman School of Medicine at the University of Pennsylvania and Penn's Abramson Cancer Center.
The findings will be presented as an oral presentation at the 62nd American Society of Hematology Annual Meeting & Exposition on Dec. 7.
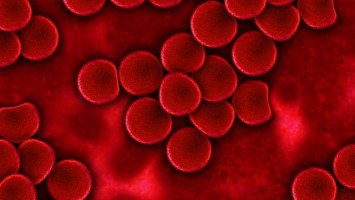
The team knocked out the CD5 gene -- which encodes for the CD5 protein on the surface of T cells and can inhibit their activation -- on CAR T cells using CRISPR-Cas9 and infused them back into mice with T- and B-cell leukaemia or lymphoma.
Mice infused with the CD5-deleted CAR T cells showed higher levels of T cell proliferation in the peripheral blood, as well as a significant reduction in tumour size and better survival outcomes compared to mice infused with non-edited CAR T cells.
CRISPR technology gives scientists the ability to locate and edit any unwanted gene.
For cancer, it works by deleting a specific gene only in T cells to help better fight tumours.
The approach is closely related to CAR T cell therapy, in which researchers collect a patient's own T cells and engineer them to express a new receptor that seeks out and attacks cancer cells.
"We've shown, for the first time, that we can successfully use CRISPR-Cas9 to knock out CD5 on a CAR T cells and enhance their ability to attack cancer," said Marco Ruella, MD, an assistant professor of Medicine in the division of Hematology-Oncology in Penn's Perelman School of Medicine and scientific director of the Lymphoma Program, who will present the results.
"The difference between edited and non-edited CAR T cells was striking in several cancer models."
The authors first tested the approach in a T-cell leukaemia model.
Anti-CD5 CAR T cells were genetically engineered to seek out CD5 on malignant T cells and attack them.
Since CD5 is also expressed on normal T cells, the authors removed it from CAR T cells, both to avoid the possible killing of other CAR T cells, and potentially to unleash CAR T cell activation that would otherwise be inhibited by the presence of CD5 on these cells.
Indeed, CD5-deleted anti-CD5 CAR T cells were significantly more potent than CAR T cells without the deletion (wild-type, CD5 ) in both in vitro and in vivo experiments, where more than 50 percent of mice were cured at long term.
To test the hypothesis that deletion of CD5 could increase the anti-tumour effect of CAR T cells targeting antigens other than CD5, the results were then validated in the setting of CTL019 CAR T cells against CD19 B-cell leukaemia.
Of note, also in this model, CD5 knockout led to significantly enhanced CTL019 CAR T cell anti-tumour efficacy with prolonged complete remissions in the majority of mice.
In a separate analysis to be shared the day of the presentation, the team reviewed a genomic database of more than 8,000 patients' tumour biopsies to study their levels of CD5 and found a correlation with outcomes.
"Basically, in most cancer types, the less CD5 expressed in T cells, the better the outcome," Ruella said. "The level of CD5 in your T cells matters."
The findings are an important step forward that may set up future clinical trials to explore how combining CAR T cell therapy and CRISPR-Cas9 gene editing could improve upon existing and new cell therapies.
Therapies such as the Penn-developed CAR T cell therapy, Kymriah (Novartis), for paediatric and adult blood cancer patients can induce dramatic responses in relapsed or refractory B-cell acute lymphoblastic leukaemia and non-Hodgkin lymphomas.
However, many patients do not respond or eventually relapse. What's more, CAR T cell therapy has not yet been proven effective in several haematological malignancies, such as T cell lymphoma and leukaemia -- blood cancers that frequently express CD5.
CD5 is also expressed in the vast majority of chronic lymphocytic leukaemia and mantle cell lymphoma patients and also in about 20 percent of acute myeloid leukaemia cases.
Today, many of the approaches to enhance CAR T therapy involve combination therapies that address T cell exhaustion, particularly the PD-L1/PD-1 axis.
This team's strategy is different in that it aims to intervene during early activation of T cells, which could open up opportunities to increase T cell function in the tumour microenvironment.
"Looking at the long term, this could represent a more universal strategy to enhance the anti-tumour effects of CAR T cells," said Carl June, MD, the Richard W. Vague Professor in Immunotherapy and director of the Center for Cellular Immunotherapies in the Abramson Cancer Center and director of the Parker Institute for Cancer Immunotherapy at the Perelman School of Medicine at the University of Pennsylvania and one of the study's authors.
"We look forward to building upon these encouraging findings in the next phase of our work."
A phase I clinical trial investigating this CD5-deleted CAR T cell approach could begin as early as 2021, the researchers said.