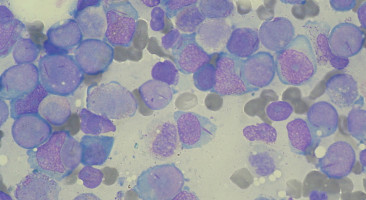
Acute myeloid leukaemia (AML) is a cancer of the blood and bone marrow that comprises 1% of all new cancer cases and almost 2% of cancer deaths in the U.S.
The five-year survival rate for the disease is less than 20%.
Researchers at the Cancer Science Institute of Singapore (CSI Singapore) at the National University of Singapore (NUS) have identified a novel molecular pathway by which a circadian clock gene, SHARP1, causes the growth of acute myeloid leukaemia (AML).
The finding paves the way for the development of new therapeutic strategies that could impede the development of this cancer of the blood and bone marrow.
The six-year long study was led by CSI director Professor Daniel Tenen, Associate Professor Reshma Taneja at the Department of Physiology, Dr. Akihiko Numata, Adjunct Research Scientist at CSI Singapore, Kwok Hui Si (a PhD student from CSI), as well as scientists from the University of Oxford, UK; the Sanford Burnham Prebys Medical Discovery Institute; the University of Alabama at Birmingham; the Medical Erasmus University Medical Center in The Netherlands; as well as the Harvard Stem Cell Institute.
It was published in the prestigious journal Nature Communications.
SHARP1 is a protein involved in the control of the circadian rhythm in humans.
Before this study, the protein had never been linked to AML.
The study focused on the role of SHARP1 in a particular subset of AML cells which contain alterations to the Mixed-Lineage Leukemia (MLL) gene.
Alteration of the MLL gene is the most common genetic occurrence leading to AML.
The alteration causes the MLL gene to fuse with other genes, thus affecting its function.
When the MLL gene combines with the AF6 gene, a "fusion" gene is created, which produces a new fusion protein called MLL-AF6.
Patients with this fusion gene tend to respond poorly to almost all types of treatment, including stem cell transplantation, and have very poor clinical outcomes.
"We found that MLL-AF6 binds with SHARP1, leading to an increase in the level of SHARP1. The increase of SHARP1 levels has the two-fold effect of initiating leukaemia development, as well as maintaining the growth of leukaemic cells. Interestingly, in addition to its own cancer-causing functions, our study also revealed that SHARP1 could act upon other target genes of MLL-AF6 to aggravate the progression of AML. But by removing or reducing the level of SHARP1, the growth of leukemic cells could be stopped, "Professor Dan Tenen explained.
The team employed an array of genetic screening techniques and cutting-edge molecular biology tools to identify the new pathway in the development of this severe type of AML. Dr Ng Chin Hin, a consultant in the Division of Haematology at the National University Cancer Institute of Singapore, said the CSI team's finding is a "truly an important discovery" that could potentially lead to drug development targeting the SHARP1-related pathway in the treatment of AML.
"AML is a deadly disease. Median survival without treatment is around 3 months, but with appropriate treatment we can cure about 30% to 40% of AML cases in those undergoing intensive chemo. At NCIS, we are seeing around 40-50 new AML cases annually, TTSH is seeing around the same figure, while SGH is higher - at 80 cases," Dr Ng added.
Source: National Univesity of Singapore