In a study published online today in Science Translational Medicine, Albert Einstein College of Medicine researchers report that an experimental peptide (small protein) drug shows promise against the often-lethal cancer acute myeloid leukaemia (AML) and describe how the drug works at the molecular level.
The findings have led to a Phase I/II clinical trial for patients with advanced AML and advanced myelodysplastic syndrome (MDS), now underway at Montefiore Health System.
In preclinical studies, the experimental drug--ALRN-6924--tripled the median survival rate in an animal model of human AML (mice transplanted with human leukaemia cells) from 50 to about 150 days.
"This is a very striking response," said study leader Ulrich Steidl, M.D., Ph.D., professor of cell biology and of medicine and the Diane and Arthur B. Belfer Faculty Scholar in Cancer Research at Einstein and associate chair for translational research in oncology at Montefiore. "Most experimental drugs for leukaemia achieve an increase in survival of only a few days in these preclinical models. Even more importantly, ALRN-6924 effectively cured about 40 percent of the treated mice, meaning they were disease free more than one year after treatment--essentially a lifetime for a mouse."
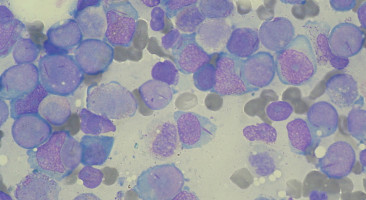
AML is caused by damage to the DNA of blood-forming stem cells in the bone marrow, resulting in abnormal white blood cells, red blood cells, or platelets.
About 21,000 people in the U.S. were diagnosed with AML in 2017.
Only 27 percent of people diagnosed with AML survive for five or more years, an outcome that has not significantly improved in the past half-century.
ALRN-6924 was developed by Aileron Therapeutics Inc. to target p53, a protein that suppresses tumours but is inactivated in many forms of cancer including AML.
The drug was designed to inhibit two naturally occurring proteins, MDMX and MDM2, whose overexpression inactivates p53, allowing cancer cells to multiply unchecked.
Aileron turned to Dr. Steidl, an AML expert, to test the drug's effectiveness in preclinical models of AML and to find out more about its mechanism of action.
Dr. Steidl and his colleagues confirmed that ALRN-6924 targets both MDMX and MDM2, blocking their interaction with p53 in AML cells.
That effect was seen in both more mature AML cells and the immature stem cells that produce them.
"This is important," said Dr. Steidl, "because AML is driven by stem cells--and if you don't target stem cells, the disease will come back very quickly."
Those same molecular changes were observed in blood cells of an AML patient who was given the drug on a compassionate-use basis. "This test was not designed to assess the efficacy of the drug in humans--that has to be done in a proper clinical trial," said Dr. Steidl. "Our goal was to determine whether it can hit the desired target in human cells in a clinical setting, which it did in this individual."
ALRN-6924 is a so-called stapled alpha-helical peptide, a promising new class of drugs whose helical structure is stabilized using hydrocarbon "staples."
The stapling prevents the peptides from being degraded by enzymes before reaching their intended target, a fate that often befalls conventional peptide drugs.
ALRN-6924 is the first stapled peptide therapeutic to be tested in patients.
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.