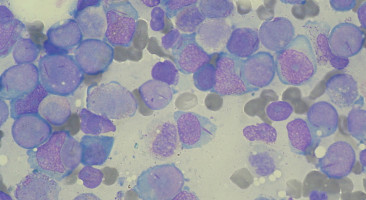
Patients whose acute myelogenous leukaemia (AML) had relapsed or was resistant to chemotherapy and those who were deemed unable to tolerate chemotherapy experienced responses to the selective BCL-2 inhibitor venetoclax (Venclexta), with complete remissions in some, according to phase II clinical trial data.
The study is published in Cancer Discovery, a journal of the American Association for Cancer Research.
Venetoclax is a small molecule that belongs to a class of drugs called BH3 mimetics.
It binds with great affinity and selectivity to BCL-2, an antiapoptotic protein that plays a role in many blood cancers, said senior author Prof Anthony Letai of the Harvard Medical School and Dana-Farber Cancer Institute.
BCL-2 proteins keep the AML cells alive by binding to proapoptotic proteins.
Venetoclax binds to BCL-2 and frees the proapoptotic proteins, thus rapidly and irreversibly forcing the AML cell to undergo apoptosis, he explained.
In April 2016, venetoclax was approved by the US Food and Drug Administration for the treatment of certain patients with chronic lymphocytic leukaemia (CLL).
The study investigators recruited 32 patients with AML with a median age of 71 years to this multicentre, single-arm trial evaluating 800 mg daily oral venetoclax.
Twenty-six patients received at least four weeks of therapy.
The investigators performed cytogenetic analysis, BH3 profiling, and next-generation sequencing to look for AML-related genetic mutations in the patients’ samples collected at study entry and found that 12 patients had mutations in IDH genes, and six had a high BCL-2-sensitive protein index.
The overall response rate was 19 percent; two patients had complete response (CR) and four had complete response with incomplete blood count recovery (CRi).
The median duration of therapy in responders was 144.5 days, and the median duration of CR was 48 days.
All patients discontinued therapy due to progressive disease or an adverse event, or for other reasons.
The four patients who had CRi had IDH mutations in their cancer cells.
Response to the drug correlated with biomarker results, including indices of BCL-2 protein expression and BH3 profiling, Letai said.
“This is significant as it supports the mechanism of action of venetoclax as an on-target inhibitor of BCL-2.
Moreover, it offers the possibility of using BH3 profiling as a potential predictive biomarker for clinical use of BH3 mimetics,” he added.
Adverse events were as expected and included nausea, diarrhoea and vomiting, febrile neutropenia, and hypokalemia.
“There has been research into apoptosis [cell death] for decades now. It has long been a goal of the field to see the work translated into actual improved care of cancer patients. AML is a disease in which new therapies are desperately needed, and based on published preclinical work, this type of cancer seemed to be an excellent target for the BCL-2 inhibitor venetoclax,” said Letai.
“In this clinical trial, we found that even among pretreated patients whose AML was refractory to intensive chemotherapy there was evidence of exceptional sensitivity to selective BCL-2 inhibition, even to the point of complete remissions. This could be accomplished by a single oral dose of venetoclax daily and demonstrated the potential clinical activity of BCL-2 inhibition in AML,” he added.
“It is also worth noting that in this age of precision medicine, dominated by genomics, this is an example of the importance of functional precision medicine. CLL and AML lack genetic abnormalities related to BCL-2. Instead, their vulnerability to BCL-2 inhibition was identified using functional studies. This is support that functional studies need to be part of any mature precision medicine project,” Letai noted.
“Marina and I both identified evidence that AML would be a good target for BCL-2 inhibition some years ago. When we realised that we were working on the same idea, we made the conscious decision to collaborate rather than compete,” Letai said.
“Combining our work made progress more rapid, and provided more material to convince AbbVie to initiate a program of venetoclax in AML.”
Lead author Prof Marina Konopleva from The University of Texas MD Anderson Cancer Center in Houston said, “We believe that venetoclax will soon become an equal partner to standard-of-care chemotherapy in elderly patients with AML when used in combinations with hypomethylating agents and other approaches. Planned studies will test the hypothesis that venetoclax may likewise improve outcomes in younger AML patients when combined with high-dose chemotherapy.”
Source: AACR
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.