Mr Masood Moghul FRCS1,2, Miss Fionnuala Croft1, Miss Fiona Mutch1, Miss Elisabeth Westaway1, Miss Amina Tran1, Miss Deokhee Yee3, Dr Patrick Kierkegaard PhD3, Netty Kinsella PhD1, Mr Declan Cahill FRCS1,2 & Professor Nicholas D James FRCR, FRCP, PhD1,2
1Department of Urology, The Royal Marsden NHS Foundation Trust, 203 Fulham Road, London, SW3 6JJ, UK
2Division of Radiotherapy and Imaging, The Institute of Cancer Research, 237 Fulham Road, London SW3 6JB, UK
3Cancer Research UK Convergence Science Centre, Imperial College London & Institute of Cancer Research, 5th floor, Roderic Hill Building, South Kensington Campus, Exhibition Road, London, SW7 2AZ
Background
Early intervention is potentially lifesaving in prostate cancer and is a major limitation of cancer outcomes with ethnicity and deprivation being determinants of inequalities that impact outcomes. The Man Van is designed to address health inequalities and barriers to accessing healthcare that affect prostate cancer with novel community-based targeting of high-risk groups using a mobile clinical unit. These inequalities are particularly relevant for men from ethnic minorities and lower socio-economic groups.
Methods
A bespoke nurse-led mobile clinical unit was moved to community-based locations in areas of high deprivation indices in London (UK) with targeted invitations to high-risk men. Men were offered prostate-specific antigen (PSA) tests and a general health check including: blood pressure, body mass index and an HbA1c test for diabetes. Phase 1 was from December 2021-December 2022 before the service streamlined and relaunched with phase 2 in January 2023.
Results
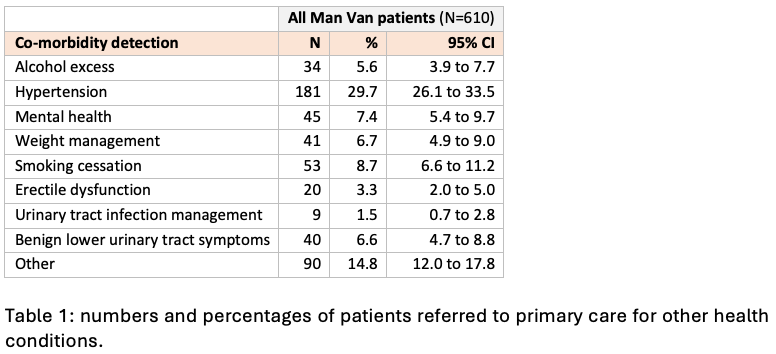
In phase 1, 610 men attended with 48% of attendees being non-White including 30% Black men. 15 prostate cancers were diagnosed (3.6%; 95% CI 2.0 to 5.9) with 10 of these being clinically significant disease. Black men were more likely to be diagnosed compared to white men: 7.1% versus 1.8% (P<0.05). 13 diabetics were diagnosed (3.9% of tests) and 50 pre-diabetics (15.1% of tests). Significant other co-morbid conditions were found as shown in table 1 below:
In phase 2, 3379 men attended (median age 59 years). 36.4% of attendees were non-White with 16.7% being Black (background 11%). 310 patients were referred for elevated PSA levels with 94 prostate cancers being diagnosed, 81 of these being clinically significant disease. The diagnostic rate of prostate cancer was 3.1%. 43 patients (2%) were diagnosed with diabetes
207 patients (11%) with pre-diabetes. No prostate cancers were metastatic at presentation, with only one being T4. 2 bladder cancers diagnosed, both high-grade and one was metastatic at presentation.
A micro-costing analysis showed costs per patient seen of £81.11 in the pilot phase, reducing by 33% to £54.32 in phase 2. Costs per-prostate cancer diagnosis were £5552.14 in the pilot reducing to £3289.81 in phase 2. A cost-consequence analysis found a 25% saving of the Man Van model versus GP model with costs-reducing from £68.41 to £51.11. A sensitivity analysis set at 20% showed that at worst the Man Van would be £6.59 more expensive than the GP model, and at best save £41.23 per patient.
Conclusions
The Man Van project is a novel approach to tackling health inequalities. Higher rates of prostate cancers were found compared with previous studies. The model offers economic value further boosted by the high levels of health conditions found. Over recruitment from ethnic minorities shows this method of outreach may be beneficial for hard-to-reach groups. While this project was conducted in a high-income country similar models can be adopted in low and middle-income countries.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.